|
Global maternity care reporting services include maternity care and delivery codes related to antepartum care, admission to the hospital for labor and delivery, management of labor (including fetal monitoring), delivery and postpartum (uncomplicated) care until six weeks postpartum. A global charge should be billed for maternity claims when all maternity-related services are provided by the same physician or physicians within the same group. Individual Evaluation and Management (E&M) codes should not be billed to report maternity visits. Prenatal care is considered part of the global reimbursement and is not reimbursed separately.
Prenatal, Delivery and/or Postpartum Services Billed Separately Only When Transfer of Care Occurs
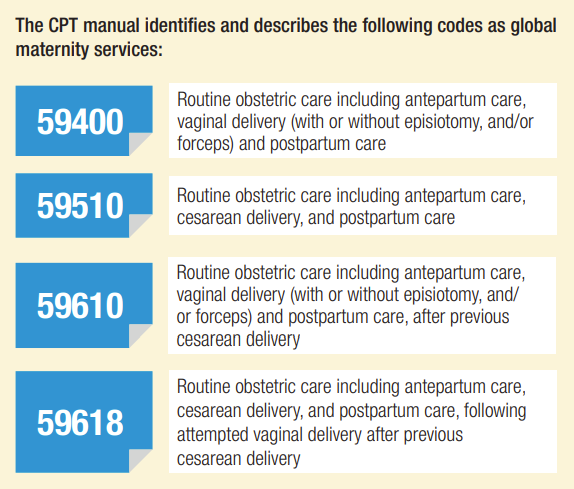
A global charge should be billed for maternity claims when all maternity-related services are provided by the same physician or physicians within the same group. Individual Evaluation and Management (E&M) codes should not be billed to report maternity visits. Prenatal care is considered part of the global reimbursement and is not reimbursed separately. The CPT manual identifies and describes the following codes as global maternity services: The following are instances where it is appropriate to submit a claim separately for prenatal, delivery and/or postpartum services:
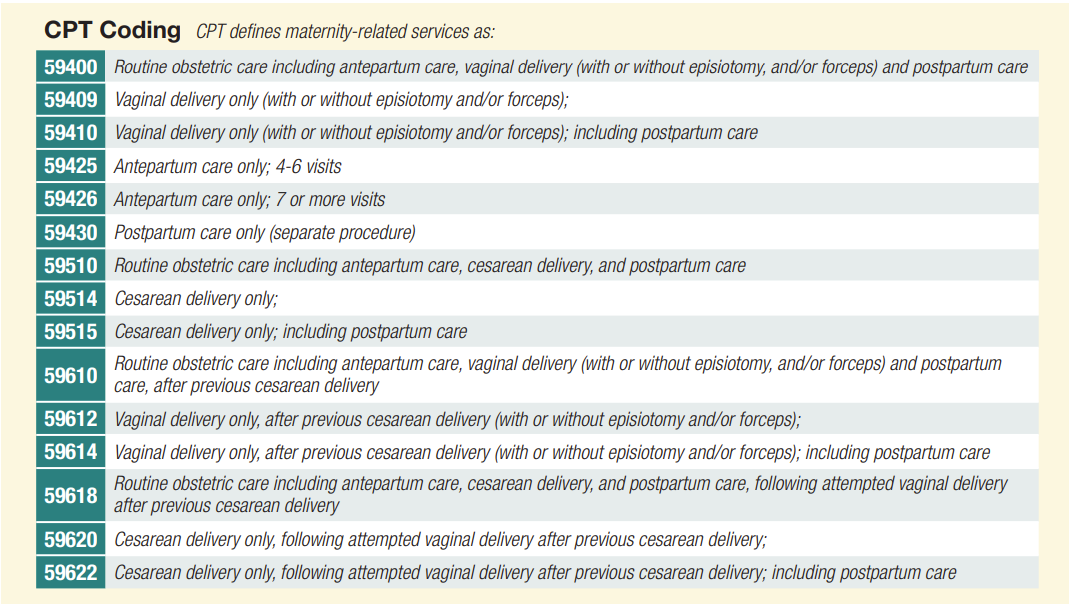
Providers should reference the Current Procedural Terminology (CPT®) manual for the most current updates and for any additional maternity related service codes. The most current codes should be submitted on a claim. Member eligibility and benefits should be determined before medical guidelines and reimbursement guidelines are applied. If a provider in a different practice provides the prenatal and/or postpartum care but does not handle the delivery, the delivering provider can file a claim using the antepartum/postpartum care only codes according to how many times the provider sees the patient. The difference between a professional fee insurance claim process and a facility fee insurance claim process is primarily in how the services provided are billed to insurance companies. Professional fee insurance claims are submitted by individual healthcare providers, such as physicians or nurse practitioners, for services they have provided to a patient. These services may include office visits, consultations, diagnostic tests, or procedures. The professional fee typically covers the cost of the healthcare provider's time and expertise.
Facility fee insurance claims, on the other hand, are submitted by healthcare facilities, such as hospitals, clinics, or ambulatory surgery centers, for services provided to a patient. These services may include the use of equipment, supplies, and staff within the facility, as well as any overhead costs associated with providing care. The facility fee covers the cost of using the facility and the associated resources. In some cases, a patient may receive both professional and facility services during a single visit, such as a surgery performed in a hospital setting. In such cases, both types of fees may be billed separately to insurance companies. It's important to note that insurance companies may have different coverage and reimbursement policies for professional and facility fees, which can impact the payment rates and amounts. Healthcare providers and facilities need to understand these policies and ensure that they are submitting accurate and appropriate claims to insurance companies to receive timely and accurate reimbursement. Understand the coding mechanics behind some of the most common obstetrical US examinations.An outsider looking in might think diagnostic radiology coding is as simple as knowing the number of views of an X-ray or whether contrast was used on a computed tomography (CT) or magnetic resonance imaging (MRI) scan. But to say that’s even the tip of the iceberg would be an understatement.
The reality is that you’ve got to be cognizant of a handful of guidelines dedicated to each diagnostic subcomponent within the radiology specialty. With the plethora of rules and guidelines to consider, obstetrical ultrasound (US) coding is almost a subspecialty in its own right. Let’s dive into the coding dynamics behind one of the many staples of diagnostic radiology coding: obstetrical US.Meet This Set of 76801 CriteriaA good chunk of diagnostic radiology coding involves using a theoretical (and sometimes literal) checklist to confirm you’ve got enough components and elements documented to achieve a given code. When it comes to obstetrical US coding, this checklist concept becomes especially important because your CPT® coding depends on it. The CPT® code book lays out a strict set of criteria necessary to reach a given obstetrical US code that varies depending on certain diagnostic components, such as trimester. Start out with a look at the criteria you’ll need to meet to report codes 76801 Ultrasound, pregnant uterus, real time with image documentation, fetal and maternal evaluation, first trimester (< 14 weeks 0 days), transabdominal approach; single or first gestation and +76802 … each additional gestation (List separately in addition to code for primary procedure):
If the report inadequately documents why one or more of the above criteria is missing, then you should either query the physician regarding an addendum or report the limited obstetrical US code 76815 Ultrasound, pregnant uterus, real time with image documentation, limited (eg, fetal heart beat, placental location, fetal position and/or qualitative amniotic fluid volume), 1 or more fetuses in place of 76801. Know When to Factor in Amniotic Fluid Assessment Determining whether the physician’s documentation meets the criteria for the assessment of amniotic fluid can be challenging. The ACR explains that “among the required elements, ‘qualitative assessment of amniotic fluid volume’ refers to the radiologist’s statement, based on his or her experience and knowledge, that the volume is adequate or inadequate.” Amniotic fluid is never mentioned on the earliest obstetrical USs of seven or eight weeks gestation because the assessment doesn’t typically become relevant until weeks 13 or 14. Most often, amniotic fluid will be evaluated and documented on the fetal anatomical structural evaluation at around 18 to 20 weeks. When providers document “no free fluid” on the seven- to eight-week fetal US, they are referring to free fluid within the peritoneal space, not amniotic fluid. Compare and Contrast 76801 With 76805 You’ll find a similar set of criteria for codes 76805 Ultrasound, pregnant uterus, real time with image documentation, fetal and maternal evaluation, after first trimester (> or = 14 weeks 0 days), transabdominal approach; single or first gestation and +76810 … each additional gestation (List separately in addition to code for primary procedure):
With respect to the “survey of intracranial/spinal/abdominal anatomy,” the ACR explains exactly what you should be looking for within the report:
Fetal Measurement Abbreviations For second and third trimester US, you’ll come across a variety of fetal measurement abbreviations included in the physician’s dictation report templates. These abbreviations and their respective measurements will act as sufficient documentation to check off a required element. Examples include:
Go a Little Further With 76805 Criteria Although amniotic fluid index (AFI) is not specifically documented as a key element, documentation should include amniotic fluid measurement with the second element for 76805: Measurements appropriate for gestational age (older than or equal to 14 weeks, 0 days). The ACR adds:After the first trimester, the amniotic fluid might be measured (quantitative), or the report may document this with a qualitative assessment — either is acceptable. If measured, this might also appear in the report simply as an abbreviation and a number. Just as you would with 76801, you may still report 76805 for an unaccounted-for element if the provider documents why the element could not be visualized or measured. If the provider fails to elaborate on the missing element, either query the physician as to whether an addendum is needed or report code 76815 instead of 76805.Other Requirements for 76811 Reporting When coding for a patient in their second or third trimester, you may have to make the distinction between a traditional US (76805) and its more detailed counterpart, 76811 Ultrasound, pregnant uterus, real time with image documentation, fetal and maternal evaluation plus detailed fetal anatomic examination, transabdominal approach; single or first gestation. This involves a thorough analysis of the dictation report. In addition to each of the elements needed to meet the requirements for 76805, the provider must also document the following to code 76811:
When discerning between 76805 and 76811, do not make a coding determination based on exam header alone. In some cases, the exam header may be formulated to state nothing more than the exam involves a 14-week or greater US examination. Outside of any extenuating circumstances, the provider usually has no need to perform a more substantial evaluation than what’s included in 76805. To qualify for 76811, the provider must document each element listed. Similar to 76805, if the provider does not document a given element, the dictation report should include a reason for non-visualization. Consider Quick Look Exam Coding Scenarios If you’re coding a report in which the provider does not document enough elements to reach the complete fetal and maternal evaluation codes, then you should resort to coding 76815. This exam is referred to as a “quick look” exam and includes one or more elements listed in the code description.The ACR elaborates a little further on code 76815: It is important to note that 76815 includes in its code description, “one or more fetuses,” and should not be coded more than once per study, or per fetus. If a study is done to reassess fetal size, or to reevaluate any fetal organ-system abnormality noted on a previous ultrasound study, 76816 is appropriate. Without a thorough examination of the report and surrounding context, it’s easy to mistakenly assign code 76815 when the documentation actually supports code 76816 Ultrasound, pregnant uterus, real time with image documentation, follow-up (eg, re-evaluation of fetal size by measuring standard growth parameters and amniotic fluid volume, re-evaluation of organ system(s) suspected or confirmed to be abnormal on a previous scan), transabdominal approach, per fetus. Begin with a few important notes offered in the CPT® code book:Code 76816 describes an examination designed to reassess fetal size and interval growth or reevaluate one or more anatomic abnormalities of a fetus previously demonstrated on ultrasound, and should be coded once for each fetus requiring reevaluation using modifier 59 for each fetus after the first. If a study is done to reassess fetal size, or to re-evaluate any fetal organ-system abnormality noted on a previous ultrasound study, 76816 is appropriate. Code This Real-World Example In the following case study, your first point of order in distinguishing between codes 76801, 76805, 76811, 76815, and 76816 is to examine the clinical indication. If the clinical indication states that it’s a follow-up obstetrical US, you need to check the patient’s chart history to determine the correct code. Keep in mind that the exam header for a fetal reassessment may look identical to that of a complete fetal and maternal evaluation as described in code 76805. Put what you’ve learned to the test by coding the following clinical example. Example: Patient admitted to emergency room (ER) for vaginal bleeding in pregnancy. A transvaginal obstetrical US is performed. The radiologist documents two subchorionic bleeds with a gestational age of eight weeks and three days. One week later, the patient presents for a first-trimester fetal and maternal US evaluation. The indication reads: “Evaluation of early pregnancy for dating. Follow-up of subchorionic hematomas.” One week following, the patient returns for a follow-up fetal and maternal US evaluation. The indication reads: “Follow-up of subchorionic hematomas.” There are more than a few instances in this patient scenario that can cause problems for a coder. The first exam is relatively straightforward. The patient presents to the ER for a transvaginal obstetrical US. Given the circumstances of this exam, you should not consider any obstetrical US code outside of 76817 Ultrasound, pregnant uterus, real time with image documentation, transvaginal. Code 76801, for instance, is a planned transabdominal procedure that involves an extra set of criteria not included in 76817. Where this situation gets tricky is when you look at the planned evaluation one week following the ER encounter. Assuming this exam at the second encounter includes all the necessary criteria to report 76801, you should code it as such. However, there’s plenty of room to get tripped up when examining the indicating diagnosis. Obstetrical radiology coders are often conditioned to see “follow-up” in the indication and immediately opt for code 76816. Evaluating the patient’s entire obstetrical examination history before making any coding considerations is always important. Looking at the bigger picture, the “follow-up” is in reference to the original ER visit, not a prior fetal and maternal evaluation exam. Since this fetal and maternal evaluation occurs at approximately nine weeks, the next point of order is to evaluate the dictation report to confirm that the exam meets all the required elements for 76801 coding. Lastly, you’ve got to make a coding determination regarding the third and final follow-up examination. Based on the clinical indication and chart history, this third examination qualifies as a true follow-up obstetrical examination. Similar to the example above, providers will routinely order these exams for patients with documented subchorionic bleeding to make sure the hematoma has not progressed. As long as this exam meets the necessary CPT® elements, you will report code 76816. https://www.aapc.com/blog/50087-master-the-art-of-obstetrical-ultrasound-coding/ As a midwife, billing can be a complicated and time-consuming process. Here are some tips to help you streamline your billing and ensure you get paid for the services you provide:
In the world of medical billing, shorter revenue cycles are crucial. Today's midwifery practices can handle more claims in less time than ever before by automating billing processes, building built-in clearinghouses with approved practice management software, and incorporating artificial intelligence into their workflows. However, not every practice is utilizing all of the technologies at its disposal, which is why we've compiled this list of the top five suggestions for accelerating billing procedures while lowering errors.
1. The Essence of Tabbing your Books The first piece of advice will improve your coding accuracy. A wonderful strategy to keep organized and productive at work is to categorize your books. One of the greatest ways to become familiar with and find the key sections of your books is to tab your code manuals. 2. Optimize your Tools In any task, having the proper tools makes a huge difference. Being a midwife biller in the modern era that still uses paper-based procedures is equivalent to being a carpenter who doesn't utilize power tools. You can automate clerical activities and fundamental billing procedures with the use of cloud-based practice management software and other medical billing software solutions, freeing up your workers' time to focus on tasks that demand a real human touch. Time will be saved, errors will be reduced, and reimbursements will be increased. 3.Increase Your Areas of Expertise You might believe you're finished if you already have the Certified Professional Coder (CPC) credential. But have you given a specialty certification any thought? This not only improves the salability of your resume but also significantly raises your earning potential. If you want to become a better medical coder, think about enrolling in a specialty certification course. 4. Prepare an Ahead-of-Time Strategy for Line or Complete Denials Millions of dollars are being unpaid as a result of increasing numbers of claims being denied. Surprisingly, however, many providers do little to recover this lost income; up to 65% of rejected claims are never resubmitted. Any billing department should make recovering this lost money a top priority, especially considering that the typical hospital has millions of dollars in unpaid claims. Ignoring these rejected claims is the same as throwing money away. Thankfully, intelligent PM software can schedule reminders for investigating refused claims and recovering lost money 5. Demand Accuracy for Coding and Claim Submission The timely submission of claims, which requires swift and precise CPT coding, is a crucial component of revenue cycle management. Effective coding procedures speed up the processing of claims and lower insurance denial rates. As it can help with code entry and automatically verify that codes have been added correctly, excellent PM software is crucial in this area as well. One of the easiest strategies to reduce denied claims and enhance your revenue cycle is to double-check everything before submitting a claim. 6. Keep an Eye on Important Statistics These days, data is key, therefore midwifery practices must monitor KPIs and other crucial information to stay in business. You should be able to view details like the processing time for claims, all denied claims, their justifications, the number of pending claims you currently have, and more. You can become more successful and efficient by better understanding the data that underlies your operation. 7. Stay Updated Finally, keep up with the market so you're the first to learn about any news or updates about medical coding. Be sure to subscribe; the Midwives Advantage blog is an excellent place to start. Another fantastic resource is the AAPC Knowledge Center. Finally, you can follow specific online personalities. The more you understand, the more distinctive you'll be as a medical coder. |
Archives
August 2023
Categories
All
|




 RSS Feed
RSS Feed